English summary: Hemispheric surgery in the treatment of severe epilepsy in children and adolescents

Background
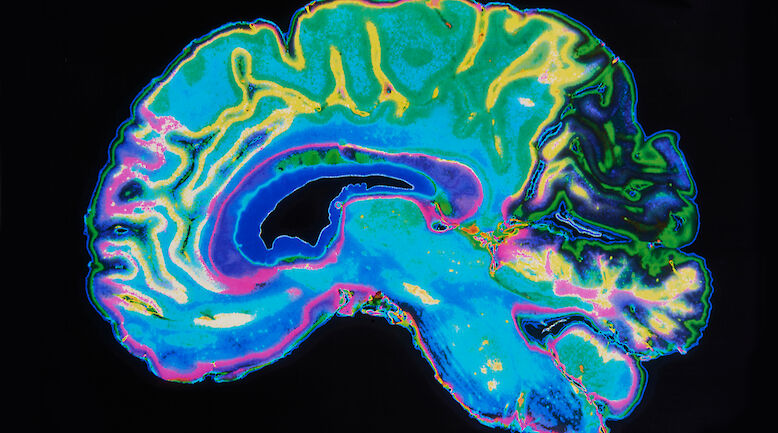
Therapy-resistant severe epilepsy with onset in childhood impairs cognitive development and increases the burden of care. Surgical treatment of epilepsy is possible if the epileptogenic area can be localized, and if its removal is not expected to cause unacceptable adverse effects. At its maximum, a resection comprises a whole hemisphere, which is nowadays usually done by disconnecting the neural pathways (i.e., hemispherotomy). Hemispheric operations have been carried out at the Helsinki University Central Hospital (HUCH) since 1991. The results of these operations have not been reported previously.
Methods
All patients who are operated for epilepsy at HUCH preoperatively undergo documentation of seizures by video-EEG, magnetic resonance imaging, evaluation of cognitive skills and have a follow-up of two years. Data on the results of these investigations, seizure onset, epilepsy syndrome, aetiology, functional status, all surgeries, postoperative outcome and complications were collected from patient charts.
Results
Hemispheric surgery was performed on 34 patients in 1991 through 2011 at a mean age of 6.8 years (range 0.4-21.2 years). The surgical method used for 88% of the patients was vertical hemispherotomy. All patients had preoperative hemiparesis. Seizure freedom was achieved after the first operation in 23 patients and after reoperation in four; altogether 27 patients (79%) became seizure free. The number of antiepileptic drugs used by the patients was considerably reduced. Ambulation was not impaired except in one patient with severe mental deficiency. Cognitive level improved in six patients (18%) and remained stable in 23 (68%), which means restoration of learning skills in patients who had had ongoing cognitive decline before the operation. Six patients (18%) required shunt placement postoperatively. Hypothalamic dysfunction was observed postoperatively in three patients (9%); this was transient in two patients and permanent in one.
Conclusions
Hemispheric epilepsy surgery renders approximately 80% of the operated patients seizure free. Control of devastating epilepsy allows the patients to resume their cognitive development. Our results are well in line with previous reports from larger epilepsy surgery centres. Vertical hemispherotomy seems to carry a risk of hypothalamic dysfunction which is usually transient. This has not been reported in association with other surgical methods. At present, epilepsy surgery is an underused treatment option in Finland. All patients with severe drug-resistant epilepsy should be evaluated for surgical treatment.